Introduction
Overview of HMPV as a Respiratory Virus
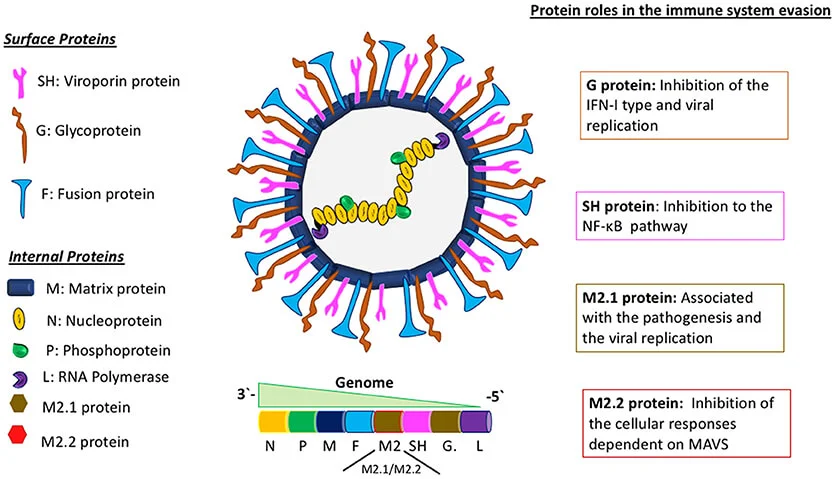
Human Metapneumovirus, classified under the Paramyxoviridae family, has garnered increasing attention due to its role as a significant etiological agent in causing acute respiratory infections. First identified in 2001, HMPV affects a broad range of individuals but is particularly problematic for vulnerable populations, including infants, the elderly, and individuals with weakened immune systems. The clinical presentation of HMPV infections spans from mild upper respiratory tract infections, such as the common cold, to severe conditions like bronchiolitis, pneumonia, and in the most extreme cases, acute respiratory distress syndrome (ARDS).
It is closely related to the Respiratory Syncytial Virus (RSV) and shares similar transmission routes, primarily via respiratory droplets or by touching surfaces contaminated with the virus. This mode of transmission facilitates the seasonal nature of the virus, with increased occurrences in colder months and during periods of heightened viral circulation. Although often underdiagnosed or misclassified as another respiratory illness due to its nonspecific symptoms, HMPV is now recognized as a significant pathogen, contributing to a notable burden on public health systems globally.
Common Symptoms Associated with HMPV Infections
Human Metapneumovirus infections are typically marked by a set of symptoms that can overlap with those caused by other common respiratory viruses, such as influenza or Respiratory Syncytial Virus (RSV). The broad range of symptoms often makes it challenging to differentiate HMPV from these other viral infections without specific testing. Here is a closer look at the most common symptoms associated with HMPV infections:
- Cough: A persistent cough is one of the hallmark symptoms of HMPV infection. This is usually dry or productive, and it can worsen as the infection progresses. The cough is often caused by inflammation and irritation of the airways as the virus replicates in the respiratory tract. This symptom can persist for several days or even weeks.
- Nasal Congestion: Nasal congestion, or stuffiness, is commonly seen in individuals with HMPV infections. This occurs as the virus infects the upper respiratory tract, leading to inflammation in the nasal passages. As a result, the individual may experience difficulty breathing through the nose, sneezing, and a runny nose.
- Pharyngitis (Sore Throat): Pharyngitis, or a sore throat, is another common symptom of HMPV. The viral infection causes inflammation in the throat, resulting in pain, discomfort, and irritation when swallowing. This can often be confused with similar symptoms seen in colds or flu.
- Fever (Pyrexia): Fever is a frequent response to HMPV infection as the body tries to fight off the virus. It is often characterized by elevated body temperature, chills, and sweating. The fever may be moderate to high and typically lasts for several days. In some cases, fever can be more pronounced in children or individuals with weakened immune systems.
- Shortness of Breath (Dyspnea): As the virus spreads deeper into the lungs, it can cause inflammation in the lower respiratory tract, leading to symptoms like shortness of breath (dyspnea). This can occur due to the narrowing of the airways or the accumulation of mucus, which can make it more difficult to breathe. Shortness of breath may be a sign that the infection is progressing to a more serious stage, such as pneumonia or bronchiolitis.
- Wheezing: Wheezing is a high-pitched sound made during breathing, often associated with airway constriction. In HMPV infections, wheezing occurs due to inflammation and obstruction in the smaller airways of the lungs. This symptom is particularly common in infants and young children, and it may indicate that the infection is causing bronchospasm or airway narrowing.

In cases where the infection progresses to more severe forms, such as pneumonia or bronchiolitis, complications like respiratory failure may develop. This could necessitate hospitalization, particularly for high-risk groups, including children under two years of age, elderly individuals, and those with underlying chronic respiratory conditions. Complications such as secondary bacterial infections and ARDS further exacerbate the severity and impact of the illness, contributing to higher morbidity and mortality rates.
Populations at Higher Risk for Severe Illness
Certain groups are more susceptible to experiencing severe outcomes from HMPV infections. These high-risk populations include:
- Infants and young children: Especially those under the age of two, who may experience significant respiratory distress.
- Elderly individuals: As they often have weakened immune responses and pre-existing chronic health conditions.
- Individuals with chronic respiratory or cardiac conditions: Those suffering from diseases like asthma, chronic obstructive pulmonary disease (COPD), or heart failure are at greater risk.
- Immunocompromised individuals: This includes patients with conditions like cancer, those on immunosuppressive treatments, or organ transplant recipients.
- Residents of congregate living settings: People living in nursing homes or long-term care facilities, where transmission is more easily facilitated, are particularly vulnerable.
These groups represent the demographic most likely to experience severe illness, highlighting the need for targeted preventive strategies, prompt diagnostic measures, and timely medical interventions to reduce the risk of complications and improve health outcomes.
Recent HMPV Outbreaks
China’s Situation
In recent months, China has witnessed a notable surge in respiratory illnesses, with hospitals in regions like Hunan province facing overwhelming patient numbers. Although many of these cases have been attributed to influenza viruses, there is growing concern regarding the potential role of HMPV, with anecdotal reports suggesting a higher prevalence than officially recognized. These reports have raised alarms about the possibility of an underreporting of HMPV infections, as health authorities continue to primarily focus on influenza. Visual evidence from social media and personal accounts of strained healthcare systems have drawn comparisons to the early days of the COVID-19 pandemic, prompting calls from health professionals for enhanced surveillance and testing for a range of respiratory pathogens, including HMPV.
International health organizations such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have advocated for increased diagnostic testing capabilities and robust public health responses. They stress the importance of tracking the spread of HMPV to understand its potential for further outbreaks, as the virus poses a significant threat to vulnerable populations, especially during seasonal respiratory virus surges.
India’s First Cases
India recently reported its first confirmed cases of HMPV, marking a significant milestone in the country’s recognition of the virus as a public health concern. These initial cases were detected in Bengaluru, involving two young children—an 8-month-old boy and a 3-month-old girl—both of whom presented with acute respiratory symptoms. The identification of these cases prompted immediate public health action, including increased surveillance in pediatric healthcare settings across the country.
The Ministry of Health and Family Welfare in India has issued guidelines for healthcare providers, stressing the importance of early identification and supportive treatment to manage the disease and prevent widespread outbreaks. As the nation’s health infrastructure continues to adapt to the challenges posed by emerging infectious diseases, the Indian government has ramped up efforts to track and contain the spread of HMPV, ensuring that timely interventions are implemented to reduce the impact of the virus.
Understanding HMPV
Discovery and History of the Virus Since 2001
It was first discovered in 2001 by Dutch researchers, although retrospective studies suggest that the virus has likely been circulating among humans for decades prior to its identification. The virus is responsible for a significant proportion of respiratory illnesses, often causing seasonal peaks in infections similar to other respiratory viruses like RSV and influenza. However, for much of its history, it was not properly identified or differentiated from other respiratory illnesses, leading to underreporting and misclassification.
HMPV infections have now been recognized worldwide, with seasonal outbreaks occurring in temperate regions during the late winter and early spring months. Its clinical features, which closely resemble those of other viral infections, have led to confusion and diagnostic challenges. Nonetheless, improved diagnostic technologies have enhanced detection capabilities, allowing for better tracking of HMPV’s impact and its spread across different regions.
Modes of Transmission
The primary modes of transmission for Human Metapneumovirus (HMPV) are important to understand in order to reduce the spread of the virus. These transmission routes include:
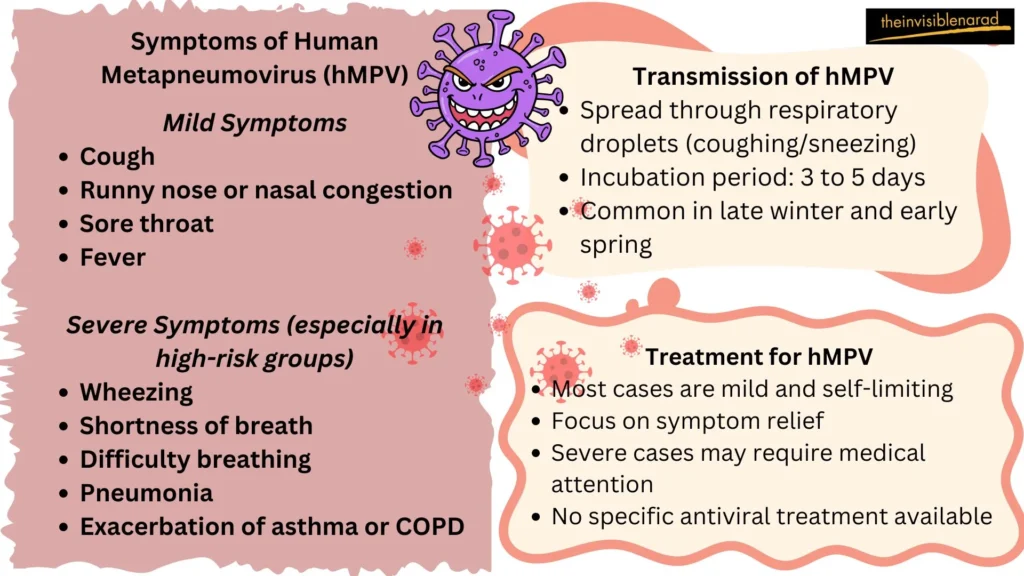
- Inhalation of Respiratory Droplets: The most common way it spreads is through the inhalation of respiratory droplets expelled by an infected individual when they cough, sneeze, or even talk. These droplets can carry the virus and travel through the air, landing on the mouths or noses of nearby individuals. The droplets can remain suspended for short periods in the air, depending on environmental factors like ventilation, making it easy for close contact settings to become breeding grounds for the virus.
- Direct Contact: Another significant route of transmission occurs when individuals come into contact with surfaces or objects that have been contaminated with it. When an infected person coughs or sneezes, the virus can settle on frequently touched surfaces such as doorknobs, light switches, and shared electronics. If a person then touches these contaminated surfaces and later touches their face, particularly the eyes, nose, or mouth, the virus can enter their body, leading to infection.
- Close Interpersonal Interactions: Close interpersonal interactions, such as handshakes, hugs, or even talking closely with an infected individual, can also facilitate the spread of HMPV. Respiratory droplets or even viral particles on the skin from direct contact can be transmitted to others. The likelihood of transmission increases significantly in settings where individuals are in close proximity for extended periods, such as in family homes, schools, or crowded public spaces.
- Aerosol Transmission: Although less common, it can also spread through fine respiratory aerosols that are created when an infected person exhales, coughs, or sneezes. These fine particles can linger in the air for longer periods than larger droplets, especially in poorly ventilated indoor environments. This type of transmission is a concern in closed settings such as hospitals, crowded indoor spaces, and public transportation. In such environments, the virus can remain suspended in the air, increasing the likelihood of exposure to people who are not in direct contact with the infected person.
- Asymptomatic Carriers: Asymptomatic individuals who carry HMPV can unknowingly contribute to the spread of the virus. These individuals may not show signs of infection, such as coughing or sneezing, but can still spread the virus to others. The presence of asymptomatic carriers complicates efforts to control outbreaks, as they might not be identified or isolated in time to prevent transmission. These individuals can still shed the virus, making it challenging to trace and contain its spread.
- Healthcare Settings: In healthcare settings, strict infection control measures are critical to prevent HMPV transmission. Healthcare workers are at increased risk of exposure due to their close contact with infected patients. The use of personal protective equipment (PPE), such as face masks, gloves, gowns, and eye protection, is essential to minimize the risk of viral transmission. Additionally, regular disinfection of medical equipment, patient rooms, and common areas, as well as limiting the movement of infected patients, are vital strategies in controlling the spread of HMPV within healthcare environments.
Given these varied modes of transmission, it is crucial to implement a multi-pronged approach to reduce the spread of HMPV. Measures such as promoting good hand hygiene, encouraging proper respiratory etiquette, maintaining physical distancing, and improving ventilation in enclosed spaces are vital to preventing outbreaks. The presence of asymptomatic carriers and aerosol transmission in specific settings highlight the need for heightened awareness and vigilance, especially in vulnerable and high-risk environments like healthcare facilities.
Similarities and Differences between HMPV and Covid-19
Human Metapneumovirus and COVID-19 are both respiratory illnesses that share certain similarities but also exhibit distinct differences.
Similarities
- Transmission: Both viruses spread primarily through respiratory droplets when an infected person coughs or sneezes. Additionally, they can be spread by touching the face after coming into contact with surfaces tainted by these droplets.
- Symptoms: Cough, fever, sore throat, nasal congestion, and dyspnea are typical symptoms. In severe cases, both can lead to pneumonia and acute respiratory distress syndrome (ARDS).
- Vulnerable Populations: Children, the elderly, and immunocompromised individuals are at higher risk for severe illness from both viruses.
Differences
- Etiology: HMPV is caused by a virus from the Paramyxoviridae family, while COVID-19 is caused by the SARS-CoV-2 virus from the Coronaviridae family.
- Vaccines and Treatments: Effective vaccines and antiviral treatments are available for COVID-19, such as Paxlovid. However, there isn’t a vaccine or particular antiviral medication for HMPV.
- Epidemiology: Infections with HMPV usually peak in late winter and early spring. COVID-19, however, has caused global pandemics with waves occurring at various times.
- Severity and Impact: While both can cause severe illness, COVID-19 has led to higher mortality rates and has had a more significant global health impact compared to HMPV.
Understanding these similarities and differences is crucial for public health strategies and individual preventive measures.
Complications of HMPV
Human Metapneumovirus is a respiratory virus that can cause mild to severe respiratory illnesses, particularly in infants, young children, the elderly, and individuals with weakened immune systems. Although the majority of HMPV infections cause only moderate respiratory symptoms, problems might happen, particularly in susceptible groups. These complications can include:
- Pneumonia: One of the most serious complications, pneumonia is an infection of the lungs that can result from an HMPV infection. It can cause difficulty breathing, chest pain, and a high fever, and may require hospitalization or intensive care.
- Bronchiolitis: HMPV is a leading cause of bronchiolitis, particularly in infants Breathing difficulties, wheezing, and coughing are symptoms of bronchiolitis, which is an inflammation and swelling of the lungs’ tiny airways. It can sometimes lead to respiratory failure in severe cases.
- Respiratory Failure: In severe cases, particularly in young children or older adults with underlying health conditions, HMPV can lead to respiratory failure. This occurs when the lungs are unable to provide enough oxygen to the blood, which can be life-threatening and require mechanical ventilation.
- Asthma Exacerbations: Individuals with pre-existing asthma may experience worsened symptoms during or after an HMPV infection. The virus can irritate the airways, leading to more frequent or severe asthma attacks.
- Croup: HMPV can cause croup, especially in young children. This condition is characterized by a distinctive cough, hoarseness, and stridor (a high-pitched sound while breathing in). In severe cases, it can lead to airway obstruction, requiring medical intervention.
- Sinusitis and Otitis Media: HMPV can also lead to secondary bacterial infections, such as sinusitis (inflammation of the sinuses) and otitis media (middle ear infections), particularly in young children.
- Dehydration: Severe respiratory illness caused by HMPV can lead to dehydration, especially in infants or elderly individuals who may have trouble drinking fluids due to illness or difficulty breathing.
- Hospitalization: Although most HMPV infections are mild, some cases can lead to hospitalization, particularly in those with weakened immune systems, the elderly, or those with pre-existing respiratory conditions. The need for hospitalization can be due to the severity of respiratory symptoms or complications like pneumonia or respiratory failure.
While HMPV is typically a self-limiting virus, these complications highlight the importance of early detection and management, particularly for those at higher risk of severe disease.
Preventive Measures to Reduce Infection Risk
Preventing the spread of Human Metapneumovirus (HMPV) involves several key strategies aimed at reducing viral transmission. These include:
- Hand Hygiene: Regular and thorough handwashing with soap and water, or using alcohol-based sanitizers, is one of the most effective ways to prevent viral spread. This practice helps eliminate viruses that may be present on the hands after touching contaminated surfaces.
- Respiratory Etiquette: Covering your nose and mouth with a tissue or your elbow when coughing or sneezing helps prevent the spread of respiratory droplets that may contain the virus. Proper disposal of used tissues and subsequent handwashing are essential to minimize transmission.
- Avoiding Close Contact with Symptomatic Individuals: Refraining from handshakes, hugs, and other close physical interactions with individuals exhibiting respiratory symptoms reduces the risk of transmission. Maintaining a safe distance from those who are sick is crucial, especially during peak seasons for respiratory viruses.
- Cleaning High-Touch Surfaces: Regularly disinfecting common areas, such as doorknobs, light switches, and shared electronics, can help minimize the risk of transmission. Using appropriate cleaning agents that are effective against viruses ensures these surfaces remain safe.
- Wearing Face Masks: In public spaces, especially during peak seasons for respiratory viruses, wearing face masks can significantly reduce the risk of transmitting HMPV and other respiratory pathogens. Proper mask usage, including hand hygiene before wearing and after removing a mask, is essential.
- Avoiding Touching the Face: Avoiding touching your face, eyes, nose, and mouth helps prevent the introduction of the virus into the body through mucous membranes. This practice is particularly important after touching potentially contaminated surfaces.
- Not Sharing Personal Items: Avoiding the sharing of food, eating utensils, or personal items with others can reduce the risk of spreading the virus. This practice helps prevent indirect transmission through contaminated objects.
- Maintaining Good Environmental Hygiene: Regularly cleaning and disinfecting frequently touched surfaces, such as furniture, toys, and commonly shared items, with appropriate cleaning agents can help minimize the risk of transmission. Maintaining good indoor ventilation and avoiding crowded or poorly ventilated public places are also important.
- Building Up Good Body Immunity: Maintaining a balanced diet, engaging in regular exercise, ensuring adequate rest, avoiding smoking, and limiting alcohol consumption can help strengthen the immune system, making it more effective in fighting off infections like HMPV.
Educational campaigns targeted at vulnerable populations and the general public can raise awareness about these preventive measures, helping to reduce the overall incidence of HMPV infections. Implementing these strategies collectively can significantly reduce the spread of HMPV and protect public health.
Conclusion
For individuals seeking to stay informed about HMPV, it is crucial to rely on trusted sources such as the WHO, CDC, and local public health departments. These organizations provide accurate, up-to-date information on the virus, preventive measures, and any evolving trends in outbreaks. Public health communication is essential in minimizing misinformation and promoting community-level adherence to health guidelines.
To reduce the risk of HMPV transmission, it is vital for individuals and communities to adhere to recommended preventive measures, such as hand hygiene, surface cleaning, and staying home when ill. By working together, healthcare providers, public health authorities, and individuals can play a significant role in controlling the spread of HMPV and other respiratory viruses, ensuring better health outcomes and minimizing the burden on healthcare systems.
Through collective action, informed public health strategies, and ongoing research, it is possible to mitigate the impact of HMPV and prepare for future outbreaks effectively.
Frequently Asked Questions (FAQs)
What is Human Metapneumovirus?
A respiratory infection called the human metapneumovirus causes a range of respiratory diseases, from minor to serious. It primarily affects young children, the elderly, and individuals with compromised immune systems, resembling other respiratory viruses such as RSV and influenza in its clinical presentation.
What are the common symptoms of HMPV infection?
Typical symptoms of an HMPV infection include:
1. Persistent cough
2. Nasal congestion
3. Sore throat (pharyngitis)
4. Elevated body temperature (fever)
5. Difficulty breathing (shortness of breath)
6. WheezingHow is HMPV transmitted?
HMPV is primarily spread through:
1. Respiratory droplets that are inhaled when an infected individual sneezes or coughs.
2. Direct contact with contaminated surfaces or items, then subsequent facial contact.
3. Close physical interactions such as handshakes or proximity during conversations.
4. Aerosolized particles in poorly ventilated indoor environments, which can facilitate the virus’s spread.Who is at higher risk for severe HMPV infection?
Those more susceptible to severe HMPV infections include:
1. Children under the age of two.
2. Older adults.
3. Individuals suffering from chronic respiratory diseases like asthma or COPD
4. People with weakened immune defensesWhat are the severe complications of HMPV?
HMPV can lead to serious health issues, including:
1. Pneumonia
2. Bronchiolitis
3. Respiratory failure
4. Secondary bacterial infections
5. Acute Respiratory Distress Syndrome (ARDS)How is HMPV diagnosed?
Diagnosis of HMPV often involves clinical evaluation supported by laboratory tests, such as PCR (Polymerase Chain Reaction) tests, which identify the virus’s genetic material in respiratory samples.
How is HMPV treated?
There is no specific antiviral treatment for HMPV. Management focuses on alleviating symptoms through rest, adequate fluid intake, and over-the-counter medications. Severe cases may necessitate hospitalization for oxygen therapy or mechanical ventilation.
Can HMPV cause repeated infections?
Yes, reinfection with HMPV is possible because immunity to the virus is not typically long-lasting. However, repeat infections tend to be less severe than the initial encounter.
How can HMPV infection be prevented?
Prevention strategies include:
1. Regular handwashing or using alcohol-based hand sanitizers.
2. Staying away from those who are exhibiting signs of respiratory infections.
3. Cleaning and disinfecting frequently touched surfaces.
4. Wearing masks in crowded areas or during peak seasons for respiratory illnesses.Is there a vaccine for HMPV?
Currently, no vaccine exists for HMPV. Prevention is mainly through good hygiene practices and adhering to infection control protocols.
