Introduction
Brief overview of Zika virus
The Zika virus, originally discovered in 1947 in the Zika Forest of Uganda, gained significant global attention in recent years due to its rapid spread and associated health concerns. The primary method of human transmission is by means of the bite of an infected Aedes mosquito, specifically Aedes aegypti and Aedes albopictus. These mosquitoes are commonly found in tropical and subtropical regions, making Zika a prevalent concern in many parts of the world.
Zika virus infection was initially considered relatively mild, with symptoms resembling those of a mild flu, including fever, rash, joint pain, and conjunctivitis. However, the virus gained notoriety due to its potential to cause serious complications, particularly in pregnant women. Zika infection during pregnancy can lead to congenital disabilities in newborns, including microcephaly and other neurological disorders.
Importance of understanding its impact
Understanding the impact of Zika virus is crucial for several reasons. Firstly, it helps individuals and communities take proactive measures to prevent infection and mitigate its spread. Given the potential for severe birth defects associated with Zika infection during pregnancy, awareness is essential for expectant mothers and those planning to conceive.
Additionally, understanding Zika’s impact is vital for healthcare professionals, policymakers, and researchers. It enables them to develop effective strategies for diagnosis, treatment, and prevention, as well as to allocate resources appropriately to address this public health threat.
Furthermore, understanding the socio-economic implications of Zika virus infection is important for vulnerable communities, as outbreaks can exacerbate existing inequalities and strain healthcare systems already facing various challenges.
Purpose of the blog post
The purpose of this blog post is to provide comprehensive information about Zika virus, including its transmission, symptoms, complications, prevention strategies, and current research developments. By offering a detailed overview of Zika, we aim to empower readers with knowledge to protect themselves and their communities, debunk common myths and misconceptions, and highlight the importance of evidence-based information in addressing public health challenges. Through this post, we hope to contribute to greater awareness and understanding of Zika virus and facilitate informed decision-making among our audience.
What is Zika Virus?
Definition and origins
Zika virus is a member of the Flaviviridae family, primarily transmitted to humans through the bite of infected Aedes mosquitoes, notably Aedes aegypti and Aedes albopictus. The virus was first identified in 1947 in the Zika Forest of Uganda, where it was isolated from a rhesus monkey. Human cases were later reported in the 1950s in Uganda and Tanzania, but the virus remained relatively obscure until outbreaks occurred in the Pacific Islands and the Americas in the 2000s and 2010s, respectively.
The name “Zika” is derived from the Zika Forest where the virus was initially discovered. Since its discovery, Zika virus has spread to various regions around the world, prompting concerns about its potential impact on public health.
Transmission pathways
Zika virus primarily spreads through the bite of infected Aedes mosquitoes, which are active during the day and often breed in standing water found in urban and suburban environments. These mosquitoes can also transmit other viruses, such as dengue and chikungunya, making them a significant public health concern in regions where they are endemic.
In addition to mosquito bites, Zika virus can also be transmitted through sexual contact, blood transfusions, and from mother to child during pregnancy or childbirth. Of particular concern is the vertical transmission of the virus from a pregnant woman to her fetus, which can result in severe birth defects and developmental abnormalities.
It’s important to note that while mosquito bites are the most common mode of transmission, other routes of transmission highlight the need for comprehensive prevention strategies and public health measures.
Global spread and affected regions
Zika virus has rapidly spread to numerous regions around the world, particularly in tropical and subtropical areas where Aedes mosquitoes thrive. Major outbreaks have been reported in various countries in Africa, Asia, the Americas, and the Pacific Islands.
One of the most significant Zika outbreaks occurred in Brazil in 2015, leading to a surge in reported cases of microcephaly and other neurological disorders in newborns. This outbreak raised global awareness of the potential consequences of Zika virus infection during pregnancy and prompted intensified efforts to control mosquito populations and prevent transmission.
While Zika virus transmission has declined in some regions since the peak of the outbreak, the risk of resurgence remains, particularly in areas with favorable environmental conditions for mosquito breeding and limited access to healthcare services. Travelers to regions with ongoing Zika transmission are advised to take precautions to prevent mosquito bites and minimize the risk of infection.
Symptoms of Zika Virus
Common symptoms
Zika virus infection often presents with mild, flu-like symptoms that typically last for a few days to a week. Common symptoms include:
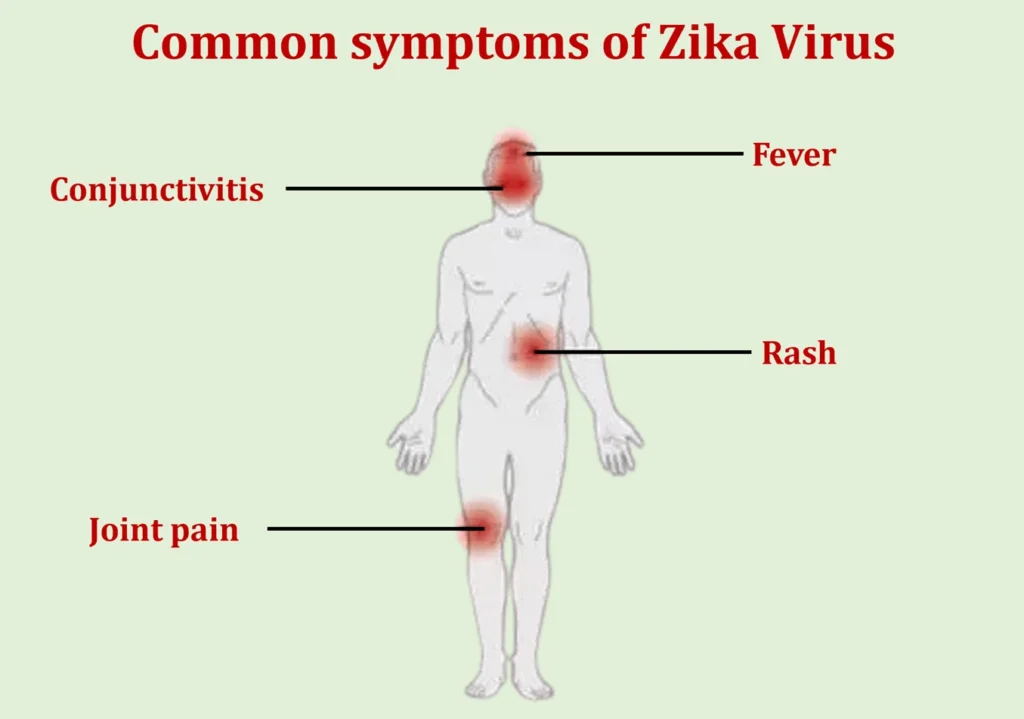
- Fever: Many individuals infected with Zika virus experience a low-grade fever, which may range from mild to moderate in intensity.
- Rash: A characteristic rash may develop shortly after the onset of fever, appearing as small red spots or raised bumps. Usually, the rash begins on the face before moving to other body areas.
- Joint pain: Zika virus infection can cause joint pain, particularly in the hands and feet. This symptom is often described as mild to moderate and may be accompanied by swelling.
- Conjunctivitis: Some individuals with Zika virus infection may experience redness and irritation of the eyes, known as conjunctivitis or “pink eye.”
It’s important to note that not all individuals infected with Zika virus will experience symptoms. In fact, the majority of cases are asymptomatic, meaning that infected individuals may not realize they have been infected.
Severity and duration
While Zika virus symptoms are generally mild and self-limiting, severe complications can occur, particularly in certain populations. In most cases, symptoms of Zika virus infection resolve within a week without medical intervention. However, some individuals may experience prolonged symptoms, such as joint pain, for several weeks or months after the initial infection.
Pregnant women infected with Zika virus are at increased risk of developing complications, including congenital disabilities in their newborns. These complications, such as microcephaly and other neurological disorders, can have long-term implications for the affected child’s health and development.
At-risk populations
While anyone can become infected with Zika virus, certain populations may be at higher risk of developing severe complications:
- Pregnant women: Zika virus infection during pregnancy poses the greatest risk, as it can lead to congenital disabilities and developmental abnormalities in the fetus, particularly if the infection occurs during the first trimester.
- Unborn babies: Infants born to mothers infected with Zika virus are at risk of congenital disabilities, including microcephaly, hearing loss, and vision problems.
- Immunocompromised individuals: People with weakened immune systems, such as those living with HIV/AIDS or undergoing immunosuppressive therapy, may be at increased risk of developing severe complications from Zika virus infection.
- Older adults: While Zika virus infection can affect individuals of all ages, older adults may be more susceptible to developing complications such as Guillain-Barré Syndrome (GBS), a rare neurological disorder associated with Zika virus infection.
Understanding the symptoms and at-risk populations associated with Zika virus infection is essential for early detection, timely medical intervention, and appropriate preventive measures, particularly for pregnant women and those planning to conceive.
Complications and Risks
Birth defects and microcephaly
- Microcephaly: One of the most concerning complications associated with Zika virus infection is microcephaly, a birth defect characterized by an abnormally small head and brain size in newborns. This condition can lead to developmental delays, intellectual disabilities, seizures, and other neurological problems. The link between Zika virus infection during pregnancy and microcephaly was first identified during the 2015 outbreak in Brazil, where a significant increase in cases of microcephaly was observed in areas with high rates of Zika virus transmission.
- Other birth defects: In addition to microcephaly, Zika virus infection during pregnancy has been linked to other congenital disabilities, including brain abnormalities, eye defects, hearing loss, and limb deformities. These birth defects can have profound and lifelong implications for affected infants and their families.
According to the Centers for Disease Control and Prevention (CDC), babies born with Zika-related birth defects may require specialized medical care and early intervention services to address their complex health needs.
Guillain-Barré Syndrome (GBS)

- Guillain-Barré Syndrome (GBS) is a rare but serious autoimmune disorder that can occur following Zika virus infection. GBS is characterized by muscle weakness, numbness, and in severe cases, paralysis. The condition occurs when the body’s immune system mistakenly attacks its peripheral nervous system, leading to nerve damage and muscle weakness.
- Association with Zika virus: While GBS can be triggered by various infections, including influenza and Campylobacter bacteria, several studies have documented an increased risk of GBS following Zika virus infection. The exact mechanism by which Zika virus contributes to the development of GBS is not fully understood, but it is believed to involve an immune-mediated response triggered by the virus. The World Health Organization (WHO) estimates that the risk of developing GBS following Zika virus infection is approximately 1 in 4,000 cases.
Long-term health implications
- Beyond the immediate complications associated with Zika virus infection, there are concerns about potential long-term health implications for both children and adults.
- Neurological consequences: Children born with Zika-related birth defects, such as microcephaly, may experience lifelong neurological challenges, including cognitive impairment, learning disabilities, and behavioral problems. Additionally, adults who develop GBS as a result of Zika virus infection may face long-term disabilities and require ongoing medical care and rehabilitation.
- Economic and social impact: The long-term health implications of Zika virus infection can place a significant burden on affected individuals, families, and healthcare systems. The cost of caring for children with Zika-related disabilities, as well as the loss of productivity due to disability or caregiving responsibilities, can have far-reaching economic and social consequences for communities affected by the virus.
According to the WHO, the economic impact of the Zika virus outbreak in Latin America and the Caribbean is estimated to be billions of dollars, including healthcare costs, lost productivity, and tourism revenue losses. Understanding the potential complications and risks associated with Zika virus infection is essential for healthcare providers, policymakers, and individuals to develop effective prevention and management strategies to mitigate the impact of the virus on public health and well-being.
Diagnosis and Testing
Clinical evaluation
- Clinical diagnosis of Zika virus infection often relies on a combination of symptoms, medical history, and epidemiological factors. Healthcare providers may consider a patient’s recent travel to regions with ongoing Zika transmission, as well as any potential exposure to mosquitoes or sexual contact with an individual known to be infected with Zika virus.
- Common symptoms of Zika virus infection, such as fever, rash, joint pain, and conjunctivitis, may prompt healthcare providers to suspect Zika as the cause of illness. However, since these symptoms are similar to those of other mosquito-borne diseases, such as dengue and chikungunya, clinical diagnosis alone may not be sufficient to confirm Zika virus infection.
Laboratory tests
- Laboratory testing is essential for confirming Zika virus infection and ruling out other possible causes of illness. The most commonly used diagnostic tests for Zika virus include molecular tests, such as reverse transcription-polymerase chain reaction (RT-PCR), and serological tests, such as enzyme-linked immunosorbent assay (ELISA) and plaque reduction neutralization test (PRNT).
- Molecular tests, such as RT-PCR, detect the presence of Zika virus RNA in blood, urine, or other bodily fluids. These tests are most reliable during the acute phase of infection when the virus is actively replicating in the body.
- Serological tests detect the presence of Zika virus-specific antibodies in the blood, which indicate a past or current infection. However, these tests may produce false-positive results due to cross-reactivity with other flaviviruses, such as dengue or yellow fever, particularly in regions where these viruses are endemic.
Challenges in diagnosis
- Cross-reactivity with other viruses: One of the main challenges in diagnosing Zika virus infection is the potential for cross-reactivity with other flaviviruses, such as dengue and yellow fever. This cross-reactivity can lead to false-positive results on serological tests, making it difficult to accurately identify Zika virus infections, especially in areas where multiple flaviviruses co-circulate.
- Limited access to testing: In some regions, access to laboratory testing for Zika virus may be limited due to resource constraints, infrastructure challenges, or delays in sample processing. This can hinder timely diagnosis and surveillance efforts, potentially contributing to underreporting of Zika virus cases and delays in public health response.
- Timing of testing: The window of opportunity for detecting Zika virus infection through laboratory testing is relatively short, as viral RNA and antibodies may only be detectable for a limited period following infection. This can make it challenging to confirm cases retrospectively, particularly if testing is delayed or if patients present with symptoms weeks or months after exposure.
According to the Centers for Disease Control and Prevention (CDC), healthcare providers should consult with state or local health departments to determine the most appropriate testing strategy for suspected cases of Zika virus infection, taking into account the individual’s symptoms, travel history, and potential exposure to the virus.
Prevention Strategies
A comprehensive approach to preventing mosquito-borne illnesses involves a combination of mosquito control measures, personal protection methods, and travel advisories. These strategies aim to mitigate the risk of transmission and reduce the incidence of diseases such as malaria, dengue fever, Zika virus, and chikungunya.
Mosquito Control Measures
- Habitat Modification: Mosquitoes breed in stagnant water, so eliminating or treating standing water sources like puddles, ponds, and water containers can significantly reduce their population.
- Insecticide Spraying: Utilizing insecticides, either through aerial spraying or targeted indoor residual spraying, can effectively kill adult mosquitoes and reduce transmission rates.
- Biological Control: Introducing natural predators of mosquitoes, such as certain species of fish or bacteria like Bacillus thuringiensis israelensis (Bti), can help control mosquito populations in bodies of water.
- Community Engagement: Educating communities about the importance of eliminating mosquito breeding sites and participating in local mosquito control efforts fosters collective action and enhances the effectiveness of prevention measures.
Personal Protection Methods
- Insect Repellents: Applying EPA-approved insect repellents containing DEET, picaridin, or oil of lemon eucalyptus on exposed skin can deter mosquitoes from biting.
- Protective Clothing: Wearing long-sleeved shirts, long pants, socks, and closed-toe shoes can reduce skin exposure and minimize the risk of mosquito bites, particularly during outdoor activities in endemic areas.
- Bed Nets: Sleeping under insecticide-treated bed nets provides an additional barrier against mosquito bites, especially in regions where mosquito-borne diseases are prevalent.
- Screening and Sealing: Installing screens on windows and doors and sealing gaps in walls and roofs helps prevent mosquitoes from entering indoor living spaces.
Travel Advisories and Precautions
- Destination-specific Guidance: Before traveling to regions with known mosquito-borne disease activity, travelers should seek advice from healthcare providers or consult reputable sources for information on recommended vaccinations, preventive medications, and current disease outbreaks.
- Timing of Travel: Avoiding peak mosquito activity periods, such as dawn and dusk, can reduce the likelihood of encountering infected mosquitoes.
- Accommodation Considerations: Choosing accommodations with air conditioning or screened windows and doors can provide additional protection against mosquito exposure during travel.
- Awareness of Symptoms: Travelers should be familiar with the symptoms of mosquito-borne diseases and seek medical attention promptly if they experience fever, headache, rash, joint pain, or other concerning symptoms, especially after returning from endemic areas.
By integrating these prevention strategies into public health initiatives, community efforts, and individual behaviors, it is possible to effectively combat the transmission of mosquito-borne illnesses and safeguard public health on a global scale.
Treatment and Management
Effective treatment and management of mosquito-borne illnesses involve a multifaceted approach tailored to the specific disease, severity of symptoms, and individual patient characteristics. This includes providing supportive care for symptomatic patients, administering antiviral therapies where applicable, and offering special recommendations for vulnerable populations such as pregnant women.
Supportive Care for Symptomatic Patients
- Fluid and Electrolyte Management: Many mosquito-borne illnesses, such as dengue fever and chikungunya, can cause dehydration due to symptoms like fever, vomiting, and diarrhea. Intravenous fluids may be necessary to maintain hydration and electrolyte balance, particularly in severe cases.
- Pain and Fever Relief: Analgesics such as acetaminophen (paracetamol) are commonly used to alleviate fever, headache, and muscle pain associated with mosquito-borne diseases. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also be prescribed but should be used cautiously, especially in cases of dengue fever, to avoid exacerbating bleeding tendencies.
- Rest and Symptom Management: Encouraging patients to rest and providing supportive care for specific symptoms, such as topical treatments for skin rashes or oral rehydration solutions for gastrointestinal symptoms, can help alleviate discomfort and promote recovery.
Antiviral Therapies
- Specific Antiviral Drugs: In the case of certain mosquito-borne viral infections like Zika virus or West Nile virus, specific antiviral medications may be under investigation or available for treatment in clinical settings. These drugs target the replication of the virus and may help reduce the duration and severity of symptoms, as well as the risk of complications.
- Experimental Treatments: Research into novel antiviral therapies for emerging mosquito-borne diseases continues to evolve. Clinical trials may offer access to experimental treatments for patients with severe or refractory cases of infection, although their efficacy and safety profiles are still being evaluated.
Recommendations for Pregnant Women
- Prenatal Screening and Monitoring: Pregnant women traveling to regions where mosquito-borne diseases are endemic should undergo pre-travel counseling and may require specialized prenatal screening for infections such as Zika virus, which can cause congenital abnormalities including microcephaly and other birth defects.
- Preventive Measures: Pregnant women are advised to strictly adhere to personal protection methods to minimize mosquito exposure, including wearing insect repellents, using bed nets, and avoiding travel to areas with active transmission of mosquito-borne diseases during pregnancy.
- Medical Consultation and Follow-up: Pregnant women who develop symptoms suggestive of mosquito-borne infections should seek prompt medical evaluation and follow-up care. Healthcare providers may recommend additional diagnostic testing, monitoring of fetal development, and supportive interventions as needed to ensure optimal maternal and neonatal outcomes.
By implementing comprehensive treatment and management strategies that address the specific needs of symptomatic patients and vulnerable populations such as pregnant women, healthcare providers can effectively mitigate the impact of mosquito-borne diseases and facilitate timely recovery and recovery.
Current Research and Developments
Continued research and development efforts are essential for advancing our understanding of mosquito-borne diseases and improving prevention, treatment, and control strategies. Key areas of focus include vaccine development, exploration of novel treatment approaches, and assessing the impact of climate change on the transmission dynamics of diseases like Zika virus.
Vaccine Development Efforts
- Dengue Fever Vaccine: Several vaccine candidates for dengue fever, a mosquito-borne viral infection endemic in tropical and subtropical regions, have been developed and are undergoing clinical trials. These vaccines aim to confer immunity against all four serotypes of the dengue virus, which can cause severe disease and hemorrhagic fever.
- Zika Virus Vaccine: Following the 2015-2016 Zika virus outbreak in the Americas, there has been significant interest in developing a vaccine to prevent Zika virus infection, particularly among pregnant women at risk of congenital Zika syndrome. Multiple vaccine candidates utilizing various platforms, including inactivated virus, DNA-based vaccines, and viral vector vaccines, are in preclinical and clinical development stages.
- Chikungunya Vaccine: Chikungunya virus, another mosquito-borne pathogen, has spurred efforts to develop a vaccine to prevent the debilitating joint pain and fever associated with the disease. Several vaccine candidates have shown promise in preclinical studies and early-phase clinical trials, with ongoing research focused on optimizing vaccine efficacy and safety.
Novel Treatment Approaches
- Antiviral Therapies: In addition to traditional antiviral drugs, researchers are exploring novel treatment approaches such as monoclonal antibodies, RNA interference (RNAi) therapeutics, and small-molecule inhibitors targeting specific stages of the viral replication cycle. These innovative therapies have the potential to enhance treatment outcomes and mitigate the emergence of drug-resistant strains.
- Host-Directed Therapies: Targeting host factors involved in the pathogenesis of mosquito-borne diseases represents another avenue for therapeutic intervention. By modulating host immune responses or cellular processes critical for viral replication, researchers aim to develop host-directed therapies that can complement antiviral drugs and improve patient outcomes.
Impact of Climate Change on Zika Transmission
- Vector Distribution and Behavior: Climate change can influence the distribution, abundance, and behavior of mosquito vectors such as Aedes aegypti and Aedes albopictus, which transmit Zika virus. Rising temperatures and altered precipitation patterns may expand the geographic range of these mosquitoes, increasing the risk of Zika transmission in previously unaffected areas.
- Epidemiological Dynamics: Changes in climate variables such as temperature and humidity can impact the seasonal patterns of mosquito activity and viral replication rates, influencing the epidemiology of Zika virus and other mosquito-borne diseases. Modeling studies are being conducted to assess the potential implications of climate change on disease transmission dynamics and guide public health interventions.
- Adaptation Strategies: To mitigate the impact of climate change on Zika transmission, adaptation strategies may include implementing vector control measures tailored to changing environmental conditions, enhancing disease surveillance and early warning systems, and promoting community engagement in mosquito bite prevention and control efforts.
By fostering collaboration between researchers, healthcare professionals, policymakers, and communities, ongoing research and development initiatives aim to accelerate progress in the prevention, treatment, and management of mosquito-borne diseases, ultimately reducing the global burden of these preventable illnesses.
Addressing Misconceptions & Myths
Misconceptions surrounding mosquito-borne diseases can lead to misinformation, fear, and ineffective prevention and treatment strategies. Addressing these misconceptions is crucial for promoting public understanding, fostering informed decision-making, and enhancing disease control efforts. This section aims to debunk common myths, clarify misconceptions about transmission, and emphasize the importance of evidence-based information.
Debunking Common Myths
Mosquitoes are attracted to certain blood types
Mosquitoes are primarily attracted to carbon dioxide, body heat, and certain chemical compounds found in sweat. Blood type does not significantly influence mosquito attraction.
All mosquitoes transmit diseases
While some species of mosquitoes are capable of transmitting pathogens like malaria, dengue virus, and Zika virus, not all mosquitoes carry disease-causing agents. Understanding the biology and behavior of different mosquito species is essential for effective vector control.
Citronella candles and wristbands provide complete protection against mosquito bites
Citronella-based products may offer limited repellent efficacy but are generally less effective than EPA-approved insect repellents containing DEET, picaridin, or oil of lemon eucalyptus. These products should be used in conjunction with other personal protection methods for optimal effectiveness.
Clarifying Misconceptions About Transmission
Mosquito-borne diseases only occur in tropical regions
While mosquito-borne diseases are more prevalent in tropical and subtropical regions with conducive climate conditions for mosquito breeding, they can also occur in temperate climates under suitable environmental circumstances. Climate change and global travel contribute to the spread of these diseases to new geographic areas.
You can only get infected with a mosquito-borne disease if you’re bitten by an infected mosquito
While mosquito bites are the primary mode of transmission for many mosquito-borne diseases, other modes of transmission may exist. For example, Zika virus can also be transmitted through sexual contact and from mother to child during pregnancy or childbirth.
Mosquito-borne diseases are untreatable and invariably fatal
While some mosquito-borne diseases can cause severe illness and complications, timely diagnosis and appropriate medical care can significantly improve patient outcomes. Antiviral drugs, supportive therapies, and preventive measures such as vaccines play essential roles in disease management and prevention.
Importance of Evidence-Based Information
- Access to Reliable Sources: In the era of widespread information dissemination through social media and the internet, it is essential to seek information from credible sources such as public health agencies, academic institutions, and reputable medical organizations. These sources provide evidence-based guidance and recommendations on mosquito-borne disease prevention, treatment, and management.
- Critical Thinking: Encouraging critical thinking and discernment of information sources helps individuals distinguish between factual information and misinformation or rumors. Fact-checking claims and consulting multiple reliable sources can aid in making informed decisions about personal health and well-being.
- Community Education and Outreach: Public health campaigns and educational initiatives play a vital role in disseminating accurate information about mosquito-borne diseases and addressing misconceptions within communities. By empowering individuals with knowledge and promoting evidence-based practices, these efforts contribute to effective disease prevention and control strategies.
By debunking myths, clarifying misconceptions, and promoting evidence-based information, stakeholders can collectively enhance public awareness, engagement, and resilience in the face of mosquito-borne disease threats, ultimately contributing to improved health outcomes and community well-being.
Community Response and Public Health Measures
Government Initiatives and Policies
Governments play a pivotal role in addressing public health crises. In response to the current situation, various government initiatives and policies have been implemented to mitigate the spread of the illness. These may include:
- Public Health Guidelines: Governments have issued comprehensive guidelines aimed at reducing transmission rates. These guidelines often encompass measures such as social distancing, mask mandates, and capacity restrictions for public gatherings.
- Vaccination Campaigns: Governments worldwide have launched extensive vaccination campaigns to inoculate their populations against the illness. These campaigns involve distribution logistics, vaccination centers, and public outreach to encourage vaccine uptake.
- Financial Support: Governments have provided economic relief packages to individuals and businesses affected by the crisis. This support aims to alleviate financial burdens and ensure the stability of essential services during challenging times.
- Travel Restrictions: Governments have implemented travel restrictions and border controls to limit the spread of the illness across regions. These measures may include quarantine requirements, testing protocols, and limitations on non-essential travel.
Role of Healthcare Professionals
Healthcare professionals are at the forefront of the response effort, providing essential medical care and expertise. Their roles include:
- Diagnosis and Treatment: Healthcare professionals diagnose cases, provide medical treatment, and offer supportive care to patients affected by the illness. This includes managing symptoms, administering medication, and monitoring patients’ progress.
- Vaccination Administration: Healthcare professionals administer vaccines as part of the vaccination campaign, ensuring that individuals receive the appropriate doses in a safe and efficient manner.
- Public Education: Healthcare professionals play a vital role in educating the public about preventive measures, vaccination benefits, and available healthcare resources. They dispel misinformation and promote evidence-based practices to empower individuals to protect themselves and others.
Importance of Public Awareness Campaigns
Public awareness campaigns are instrumental in fostering community engagement and encouraging adherence to public health guidelines. These campaigns aim to:
- Disseminate Information: Public awareness campaigns disseminate accurate information about the illness, its transmission, and preventive measures. They address common misconceptions and provide clear guidance on how individuals can protect themselves and others.
- Promote Behavioral Change: By raising awareness about the importance of preventive measures such as hand hygiene, mask-wearing, and vaccination, these campaigns seek to influence individual behavior positively. They emphasize collective responsibility and the role each person plays in controlling the spread of the illness.
- Combat Stigma: Public awareness campaigns combat stigma and discrimination associated with the illness. They promote empathy, solidarity, and understanding, fostering a supportive environment for affected individuals and communities.
Conclusion & FAQs
In summary, effective community response and public health measures are essential for mitigating the impact of the current public health crisis. Government initiatives, the dedication of healthcare professionals, and public awareness campaigns all play critical roles in this effort.
Moving forward, it is imperative that individuals continue to adhere to public health guidelines, get vaccinated, and stay informed about the latest developments. Community engagement and collective action are crucial for preventing further spread and protecting vulnerable populations.
While the current situation presents significant challenges, there is optimism for the future. Through continued collaboration, innovation, and global solidarity, we can overcome this crisis and work towards the eradication of the illness. Together, we can build a healthier and more resilient world for future generations.
Frequently Asked Questions (FAQs)
What is Zika virus and how is it transmitted?
Zika virus is a mosquito-borne virus primarily transmitted to humans through the bite of infected Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus. It can also be transmitted through sexual contact, blood transfusion, and from mother to fetus during pregnancy.
What are the symptoms of Zika virus infection?
Many Zika virus-infected individuals do not show any symptoms. However, fever, rash, headache, muscular soreness, joint discomfort, and conjunctivitis (red eyes) are typical symptoms. Usually minor, the symptoms can linger for a few days to a week.
How is Zika virus diagnosed?
Zika virus infection can be diagnosed through laboratory tests, including reverse transcription-polymerase chain reaction (RT-PCR) to detect the virus’s genetic material or serological tests to detect antibodies produced by the body in response to the virus.
Is there a treatment for Zika virus infection?
There is no specific antiviral treatment for Zika virus infection. Treatment primarily focuses on relieving symptoms, such as rest, hydration, and pain relief medication (e.g., acetaminophen). Individuals with Zika virus infection should avoid aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) until dengue fever is ruled out to reduce the risk of bleeding complications.
Can Zika virus infection cause complications?
In most cases, Zika virus infection causes mild symptoms. However, it can lead to severe complications, especially in pregnant women. Zika virus infection during pregnancy is associated with an increased risk of birth defects, including microcephaly (abnormally small head size) and other neurological abnormalities in infants.
Is it safe to travel to areas with Zika virus transmission?
Travelers, especially pregnant women and couples planning pregnancy, should consult healthcare providers and consider the risks associated with Zika virus transmission in their destination. They should follow preventive measures to avoid mosquito bites and practice safe sex during travel and for some time after returning to prevent potential transmission.
Is there a vaccine available for Zika virus?
As of now, there is no licensed vaccine available for Zika virus. However, research and development efforts are ongoing to develop vaccines and other preventive measures against Zika virus infection.
Where can I find more information about Zika virus?
Reliable sources of information about Zika virus include national and international public health agencies, such as the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and local health departments. These organizations provide updated guidelines, travel advisories, and resources for healthcare professionals and the public.
