Introduction
Brief Overview of Mumps and Its Resurgence in Recent Years
Mumps, a viral infection characterized by painful swelling of the salivary glands, has made a concerning resurgence in recent years, despite being largely preventable. While once considered a childhood rite of passage, its outbreaks have reappeared with alarming frequency, affecting individuals of all ages.
In a recent surge, Kerala (India) grapples with a concerning its outbreak, registering a staggering 190 cases in a single day on March 10th,2024. This alarming spike has prompted swift action, with authorities from the Union Health Ministry confirming the alert to the National Centre for Disease Control.
The escalation in cases follows a notable trend, as the state had already reported over 2,500 cases the previous month. Kerala’s struggle with mumps mirrors similar challenges faced in various other regions across the country. Instances of its outbreaks have surfaced in states like Maharashtra, Andhra Pradesh, and Telangana, causing growing unease among parents and healthcare professionals alike. This resurgence has sparked renewed interest in understanding the causes, symptoms, and prevention strategies surrounding this infectious disease.
Importance of Awareness and Understanding for Effective Prevention and Management
In the face of mumps resurgence, raising awareness and fostering understanding about the virus are crucial for effective prevention and management. With the right information, individuals can take proactive measures to protect themselves and their communities, while healthcare professionals can swiftly diagnose and treat cases to prevent further spread.
What is Mumps?
Definition of Mumps: A Contagious Viral Infection
Being highly contagious viral infection it is primarily affects the salivary glands, leading to painful swelling, particularly of the parotid glands located on the sides of the face. However, it can also cause a range of other symptoms and complications, making it more than just a benign childhood illness.
Historical Context: Past Outbreaks and Vaccination Efforts
It has a long history of causing outbreaks, with documented cases dating back centuries. However, significant strides in vaccination efforts, particularly with the introduction of the MMR (Measles, Mumps, Rubella) vaccine, led to a dramatic decline in its cases in the latter half of the 20th century. Unfortunately, recent years have seen a resurgence of mumps outbreaks in various parts of the world, challenging the effectiveness of vaccination campaigns and highlighting the need for ongoing vigilance.
Overview of the Causative Agent: The Mumps Virus
Belonging to the Paramyxoviridae family, the mumps virus stands among distinguished company within its viral relatives. This encompassing family includes various genera, each with its unique viral members:
- Rubulavirus: This genus hosts not only the mumps virus but also notable counterparts such as the New Castle disease virus and human parainfluenza virus types 2, 4a, and 4b.
- Paramyxovirus: Among its members are human parainfluenza virus types 1 and 3, contributing to the diversity of this viral genus.
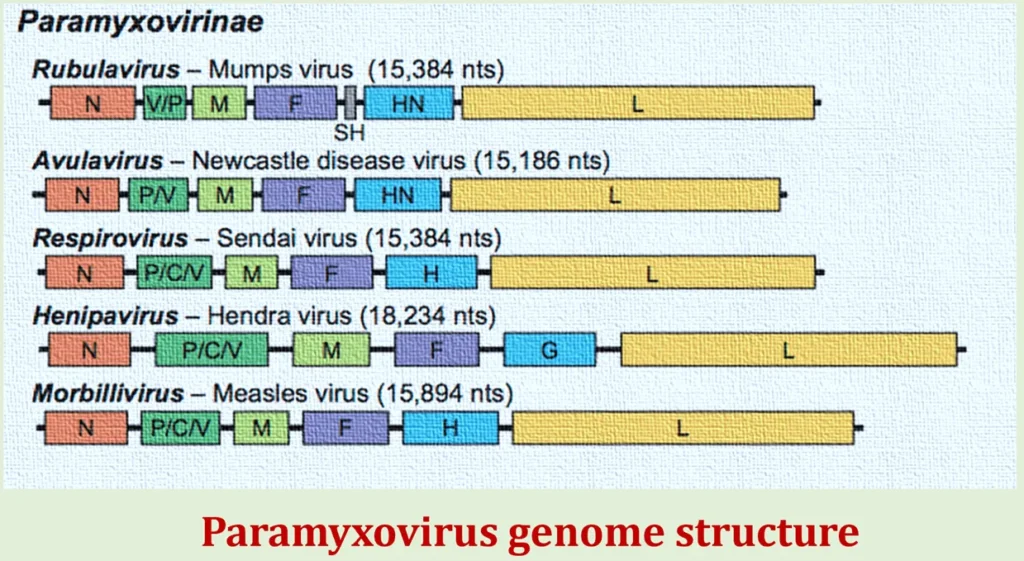
- Morbillivirus: Recognizable for its notorious representative, the measles virus, this genus evokes significant public health concerns globally.
- Pneumovirus: Completing the roster is the human respiratory syncytial virus, a leading cause of respiratory tract infections in both children and adults.
The discovery of this virus dates back to 1934 when Johnson and Goodpasture first identified this viral agent, marking a pivotal moment in the understanding of infectious diseases. It is a single-stranded RNA virus that primarily spreads through respiratory droplets from coughing, sneezing, or talking, as well as through direct contact with infected saliva. The virus can survive on surfaces for several hours, making transmission relatively easy, especially in crowded settings.
Understanding the nature of the mumps virus, its modes of transmission, and its historical context is essential for developing effective prevention and control strategies. In the subsequent sections of this article, we will delve deeper into the signs and symptoms of it, its diagnosis and treatment, as well as prevention strategies aimed at curbing its spread and mitigating its impact on public health.
Causes and Transmission
How the Mumps Virus Spreads?
This virus spreads primarily through respiratory droplets expelled when an infected person coughs, sneezes, or talks. These droplets can land on surfaces or be inhaled by individuals in close proximity, facilitating transmission. Additionally, the virus can spread through direct contact with infected saliva, such as sharing utensils or kissing an infected person.
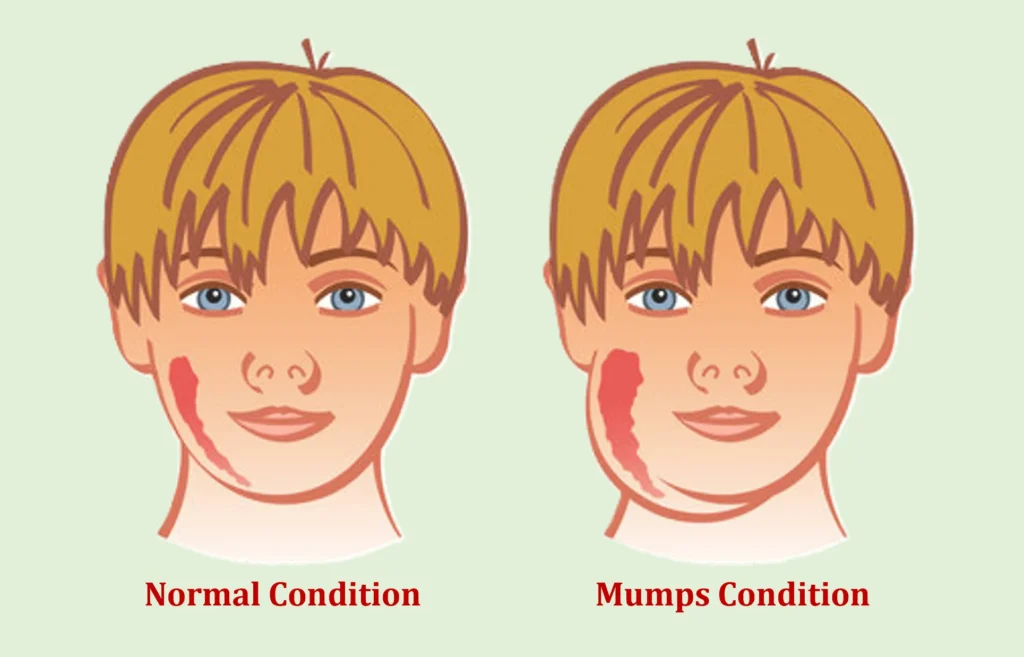
Once the virus enters the body, it replicates in the upper respiratory tract and spreads to other tissues, including the salivary glands, where it causes inflammation and swelling. This swelling of the salivary glands, particularly the parotid glands located on the sides of the face, is characteristic of its infection.
Factors Contributing to Transmission
Several factors contribute to the transmission of the mumps virus, including:
- Crowded Environments: Settings with close contact among individuals, such as schools, colleges, dormitories, and childcare facilities, provide ideal conditions for the spread of it.
- Low Vaccination Rates: Inadequate vaccination coverage within communities increases the likelihood of its outbreaks. Individuals who are unvaccinated or under-vaccinated are at higher risk of infection and can serve as reservoirs for the virus.
- Lack of Immunity: Immunity to it can wane over time, leaving previously vaccinated individuals susceptible to infection, especially in areas where its circulation is high.
- Asymptomatic Transmission: Some individuals infected with this virus may not exhibit symptoms (asymptomatic carriers) but can still spread the virus to others, unknowingly contributing to transmission.
Incubation Period and Contagiousness
The incubation period for mumps—the time between exposure to the virus and the onset of symptoms—typically ranges from 12 to 25 days, with an average of 16 to 18 days. During this period, infected individuals may not show any symptoms but can still spread the virus to others.
Contagiousness peaks shortly before the onset of symptoms and persists for several days afterward. Infected individuals remain contagious for about five days after the onset of parotitis, although the virus can be shed in saliva for up to two weeks or longer in some cases. This prolonged shedding period underscores the importance of isolation and infection control measures to prevent further transmission.
Understanding how the mumps virus spreads and the factors that contribute to transmission is essential for implementing effective control measures and preventing outbreaks. In the next section, we will explore the signs and symptoms of mumps, as well as the potential complications associated with the infection.
Signs and Symptoms
Common Symptoms
It typically manifests with a distinct set of symptoms, although the severity can vary among individuals. Common symptoms of it include:
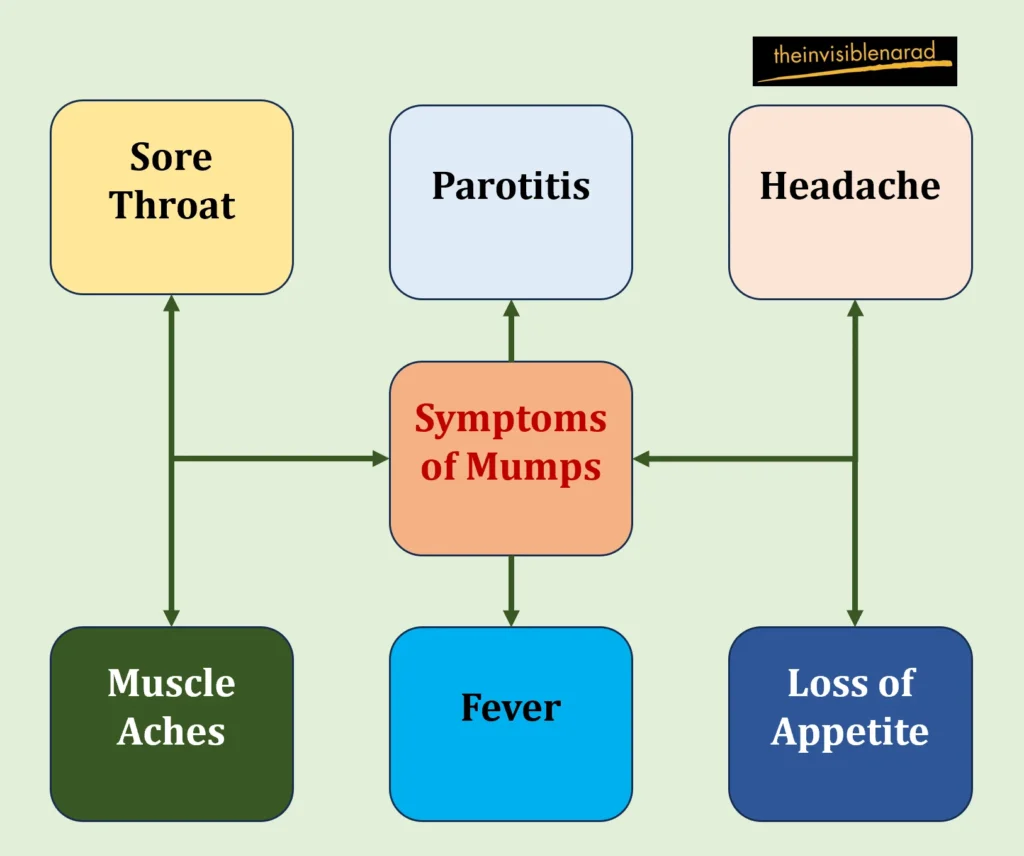
- Parotitis: Swelling and tenderness of one or both parotid glands, which are located just below and in front of the ears. This swelling gives the cheeks a characteristic “chipmunk” appearance and can be accompanied by pain while chewing or swallowing.
- Fever: Many individuals with this experience a low-grade fever, usually ranging from 100.4°F (38°C) to 104°F (40°C). Fever may precede or coincide with the onset of parotitis.
- Headache: Headaches are common during this infection and may range from mild to severe.
- Muscle Aches: Generalized muscle aches and fatigue are often reported, contributing to overall discomfort.
- Loss of Appetite: Some individuals with it may experience a decreased appetite, possibly due to pain while eating.
- Sore Throat: Inflammation of the salivary glands can lead to a sore throat, especially when swallowing.
While these symptoms are characteristic of mumps, it’s important to note that not all infected individuals will experience all of these symptoms. Some may exhibit mild symptoms or remain asymptomatic altogether, particularly in young children.
Complications
While it is typically a self-limiting illness, it can lead to complications, especially in adolescents and adults. Complications of it may include:
- Meningitis: One of the possible side effects of having the it is inflammation of the meninges, which are the membranes that coat the brain and spinal cord. Symptoms of meningitis include light sensitivity, stiff neck, and excruciating headaches.
- Encephalitis: It can occasionally lead to encephalitis, a rare but serious complication characterized by inflammation of the brain tissue. Encephalitis may cause symptoms such as confusion, seizures, and impaired consciousness.
- Orchitis: Orchitis, or swelling of the testicles, is a common complication of it in post-pubertal males. It can cause pain, swelling, and tenderness in one or both testicles and may lead to infertility in rare cases.
- Oophoritis: Oophoritis, inflammation of the ovaries, can occur as a complication of it in females. It may cause abdominal pain, fever, and menstrual irregularities.
- Deafness: Rarely, its infection can lead to permanent hearing loss, particularly if the virus affects the auditory nerve or causes damage to the structures of the inner ear.
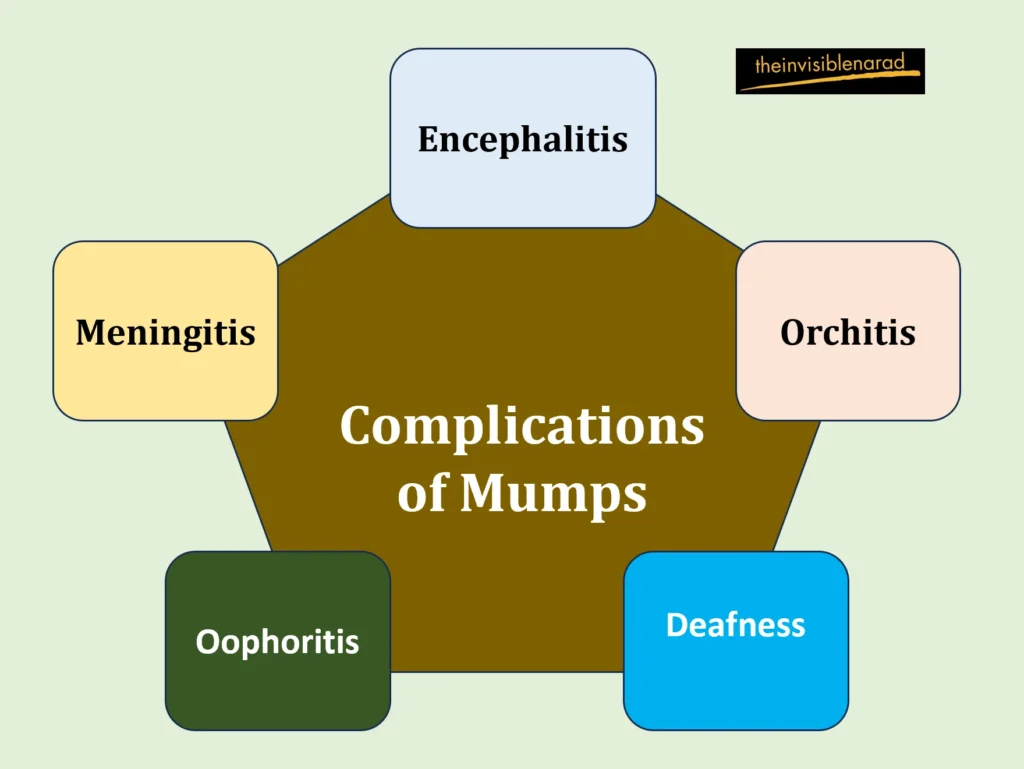
While these complications are relatively rare, they underscore the importance of timely diagnosis and appropriate management of mumps infections.
Variances in Symptom Severity Among Different Age Groups
The severity of mumps symptoms can vary among different age groups. In general:
- Children: Children infected with this infection may exhibit milder symptoms compared to adolescents and adults. They may also be less likely to experience complications such as orchitis and oophoritis.
- Adolescents and Adults: Adolescents and adults are more likely to experience severe symptoms and complications of it, including parotitis, meningitis, and orchitis. This age group may also have a higher risk of developing long-term complications such as deafness.
Understanding the potential complications of it and the variations in symptom severity among different age groups is essential for accurate diagnosis and appropriate management. In the next section, we will explore the diagnostic methods and treatment options available for it.
Diagnosis and Treatment
Diagnostic Methods
- Clinical Examination: A healthcare provider will typically perform a physical examination to assess for characteristic signs of it, such as swelling of the parotid glands. The presence of bilateral or unilateral swelling, along with other symptoms like fever and sore throat, may strongly suggest a diagnosis of mumps.
- Laboratory Tests
- Viral Culture: A viral culture involves collecting a sample of saliva or swabbing the inside of the cheek to detect the presence of this virus. However, viral culture may take several days to yield results and is less commonly used compared to other diagnostic methods.
- Serology: Serological tests, such as enzyme-linked immunosorbent assay (ELISA) or neutralization assays, can detect the presence of antibodies specific to this virus in the blood. These tests are useful for confirming a diagnosis of it, especially when performed during the acute phase of infection.
Supportive Care
While there is no specific antiviral treatment for mumps, supportive care can help alleviate symptoms and promote recovery. Supportive measures may include:
- Rest: Encouraging adequate rest allows the body to focus its energy on fighting off the infection and promotes faster recovery.
- Hydration: Drinking plenty of fluids helps prevent dehydration, especially if fever is present. Water, herbal teas, and clear broth are good choices.
- Pain Management: Over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help alleviate fever, headache, and muscle aches associated with it. Aspirin should be avoided in children and adolescents due to the risk of Reye’s syndrome.
Importance of Early Diagnosis and Management to Prevent Complications
Early diagnosis and prompt management of mumps are crucial for preventing complications and reducing the risk of transmission to others. Timely diagnosis allows for appropriate supportive care measures to be implemented, which can help alleviate symptoms and promote a smoother recovery.
Moreover, early identification of its cases enables healthcare providers to implement infection control measures to prevent further spread of the virus. Isolation of infected individuals, especially in communal settings such as schools and daycare centers, can help contain outbreaks and protect vulnerable populations, including those who are unvaccinated or immunocompromised.
In addition to mitigating the immediate impact of mumps infection, early diagnosis and management also play a critical role in preventing long-term complications such as meningitis, orchitis, and deafness. By promptly identifying and treating cases of mumps, healthcare providers can minimize the risk of severe outcomes and promote the overall well-being of affected individuals.
Early diagnosis and appropriate supportive care are essential components of mumps management, emphasizing the importance of timely healthcare intervention in mitigating the impact of this infectious disease.
Prevention Strategies
Mumps is a highly contagious viral infection, but it can be effectively prevented through various strategies. In this section, we will explore key prevention methods, including vaccination, herd immunity, and additional preventive measures.
Vaccination: The Key to Mumps Prevention
Vaccination is the cornerstone of mumps prevention. The MMR (Measles, Mumps, Rubella) vaccine is highly effective in preventing mumps infection, and it is routinely administered to children in many countries as part of their childhood immunization schedule. The vaccine contains live attenuated viruses that stimulate the immune system to produce protective antibodies against mumps, measles, and rubella.

Routine vaccination with two doses of the MMR vaccine, typically given at 12-15 months and 4-6 years of age, provides long-lasting immunity to mumps in the majority of individuals. However, in cases of outbreaks or high-risk exposures, additional doses of the vaccine may be recommended by public health authorities.
Vaccine Efficacy and Safety
The MMR vaccine has been extensively studied and proven to be safe and effective in preventing mumps infection. Clinical trials have demonstrated high levels of vaccine efficacy, with two doses providing approximately 88% protection against mumps.
Serious adverse reactions to the MMR vaccine are rare, with the benefits of vaccination far outweighing the risks. Common side effects, such as mild fever, rash, or temporary pain at the injection site, are typically mild and transient.
It’s important to address concerns or misconceptions about vaccine safety through education and evidence-based information, as vaccine hesitancy can contribute to suboptimal vaccination coverage and increase the risk of mumps outbreaks.
Herd Immunity and Its Role in Preventing Outbreaks
Herd immunity, also known as community immunity, occurs when a significant proportion of the population is immune to a contagious disease, either through vaccination or prior infection. Herd immunity plays a crucial role in preventing outbreaks by reducing the overall transmission of the virus within a community.
Maintaining high vaccination coverage rates is essential for achieving herd immunity against mumps. When a sufficient percentage of the population is vaccinated, the virus has fewer opportunities to spread, protecting vulnerable individuals who cannot be vaccinated due to medical reasons or age.
Other Preventive Measures
In addition to vaccination, several other preventive measures can help reduce the risk of mumps transmission:
- Hand Hygiene: Regular handwashing with soap and water, especially after coughing, sneezing, or touching potentially contaminated surfaces, can help prevent the spread of mumps and other infectious diseases.
- Respiratory Etiquette: Covering coughs and sneezes with a tissue or the elbow can minimize the release of respiratory droplets containing the mumps virus into the air.
- Avoiding Close Contact with Infected Individuals: Individuals diagnosed with mumps should be isolated from others, especially in settings where close contact is common, such as schools or workplaces, until they are no longer contagious.
By implementing comprehensive prevention strategies, including vaccination, promotion of herd immunity, and adherence to preventive measures such as hand hygiene and respiratory etiquette, the incidence of mumps can be significantly reduced, contributing to the overall improvement of public health.
Treatment and Management of Mumps
Mumps is typically a self-limiting illness, meaning it resolves on its own without specific medical treatment in most cases. However, supportive care and management strategies can help alleviate symptoms, prevent complications, and reduce the risk of transmission to others. In this section, we will explore medical treatments, home remedies, and the necessity of isolation for mumps patients.

Medical Treatments for Mumps
- Pain Relief: Over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help reduce fever and alleviate pain associated with mumps, such as headache or swollen glands. Aspirin should be avoided in children and adolescents due to the risk of Reye’s syndrome.
- Hydration: Drinking plenty of fluids, such as water, herbal teas, or clear soups, is important to prevent dehydration, especially if fever is present. Fluid intake should be increased if swallowing is difficult due to swollen glands.
- Rest: Getting plenty of rest allows the body to conserve energy and focus on fighting the mumps virus. Bed rest may be necessary, particularly during the acute phase of illness when symptoms are most severe.
- Antibiotics: Antibiotics are not effective against viral infections like mumps and are not routinely prescribed unless there is a secondary bacterial infection, such as bacterial meningitis.
- Antiviral Medications: There are no specific antiviral medications available for the treatment of mumps. Supportive care is still the cornerstone of caregiving.
Home Remedies for Easing Mumps Symptoms
- Warm or Cold Compresses: Applying a warm or cold compress to swollen glands can help reduce inflammation and alleviate pain. Use caution to avoid extreme temperatures that may cause skin irritation.
- Soft Diet: Consuming soft foods that are easy to chew and swallow, such as mashed potatoes, yogurt, or smoothies, can help minimize discomfort while eating.
- Gargling with Salt Water: Gargling with warm salt water may help soothe a sore throat and reduce inflammation in the mouth and throat.
- Steam Inhalation: Inhaling steam from a bowl of hot water or taking a steamy shower can help relieve congestion and ease breathing, especially if nasal congestion is present.
- Herbal Remedies: Some individuals find relief from mumps symptoms by using herbal remedies such as ginger, chamomile, or licorice root. However, it’s important to consult with a healthcare professional before using herbal supplements, especially in children or individuals with underlying health conditions.
Is Isolation Necessary for Mumps Patients?
Isolation of mumps patients is recommended to prevent the spread of the virus to others, especially in settings where close contact is common, such as schools, childcare facilities, or healthcare settings. The contagious period for mumps begins several days before the onset of symptoms and lasts for about five days after the onset of parotitis.
During the contagious period, mumps patients should avoid close contact with others, including staying home from school or work and avoiding social gatherings. They should also practice good respiratory hygiene by covering coughs and sneezes with a tissue or the elbow and regularly washing hands with soap and water.
Isolation precautions may vary depending on local public health guidelines and the severity of the outbreak. Close contacts of mumps patients, particularly those who are unvaccinated or at high risk of complications, may be advised to receive post-exposure prophylaxis or to monitor for symptoms and seek medical attention if they develop signs of mumps infection.
While there is no specific treatment for mumps, supportive care, home remedies, and isolation precautions can help manage symptoms, prevent complications, and reduce the risk of transmission to others. Individuals with mumps should consult with a healthcare professional for appropriate management and follow public health recommendations to minimize the spread of the virus within their communities.
Mumps in the Modern Era
Recent Trends in Mumps Outbreaks
Despite the availability of a highly effective vaccine, mumps outbreaks have resurged in various parts of the world in recent years. These outbreaks represent a significant public health concern and highlight the ongoing challenges in controlling the spread of this contagious viral infection. Recent trends in mumps outbreaks include:
- Increased Incidence: Many countries have reported an increase in the number of mumps cases, with outbreaks occurring in communities, schools, universities, and other settings where individuals are in close contact.
- Diverse Geographical Distribution: Mumps outbreaks have been observed in both developed and developing countries, indicating that the resurgence of the virus is not limited to specific regions or socioeconomic contexts.
- Age Distribution: While mumps primarily affects children, recent outbreaks have also affected adolescents and young adults, highlighting the importance of vaccination across all age groups.
- Epidemiological Patterns: Outbreaks often occur in settings with suboptimal vaccination coverage, allowing the virus to spread rapidly among susceptible individuals. Close-contact environments such as schools, dormitories, and healthcare facilities are particularly susceptible to mumps transmission.
Challenges in Maintaining Vaccination Coverage
Despite the availability of a safe and effective vaccine, maintaining high vaccination coverage rates remains a challenge in many regions. Several factors contribute to challenges in maintaining vaccination coverage for mumps:
- Vaccine Hesitancy: Vaccine hesitancy, fueled by misinformation and misconceptions about vaccine safety and efficacy, has led to a decline in public confidence in vaccination programs. Some individuals or communities may delay or refuse vaccination, increasing the risk of mumps outbreaks.
- Access Barriers: Socioeconomic factors, including poverty, lack of access to healthcare services, and geographic isolation, can create barriers to vaccination for certain populations, leading to disparities in vaccination coverage.
- Logistical Challenges: Ensuring access to vaccines and maintaining cold chain storage infrastructure can be challenging, particularly in remote or underserved areas with limited healthcare resources.
- Complacency: In regions where mumps is relatively rare or outbreaks have not occurred recently, complacency about vaccination may arise, leading to decreased demand for vaccination services and suboptimal coverage rates.
Impact of Misinformation and Vaccine Hesitancy
Misinformation and vaccine hesitancy have a significant impact on vaccination uptake and coverage rates, contributing to mumps outbreaks and undermining public health efforts to control the spread of the virus. The impact of misinformation and vaccine hesitancy includes:
- Decline in Vaccination Rates: Misinformation about vaccines, including false claims linking vaccines to autism or other adverse effects, can lead to a decline in vaccination rates, leaving populations vulnerable to mumps and other vaccine-preventable diseases.
- Erosion of Public Trust: The spread of misinformation erodes public trust in vaccination programs and healthcare authorities, making it more challenging to effectively communicate accurate information about vaccines and their importance for public health.
- Risk of Outbreaks: Vaccine hesitancy increases the risk of mumps outbreaks by reducing overall vaccination coverage and herd immunity within communities, allowing the virus to circulate more freely and infect susceptible individuals.
- Health Disparities: Vaccine hesitancy disproportionately affects marginalized or vulnerable populations, exacerbating existing health disparities and inequalities in access to healthcare services.
Public Health Responses and Strategies for Outbreak Control
Public health responses to mumps outbreaks require a coordinated effort involving healthcare providers, public health agencies, policymakers, and community stakeholders. Key strategies for outbreak control include:
- Surveillance and Monitoring: Timely detection and reporting of mumps cases through surveillance systems enable public health authorities to monitor trends, identify outbreaks, and implement targeted interventions.
- Vaccination Campaigns: Intensified vaccination campaigns targeting affected populations, including catch-up vaccination for individuals who are unvaccinated or under-vaccinated, can help contain outbreaks and prevent further transmission.
- Public Education and Communication: Public awareness campaigns and educational initiatives play a crucial role in combating misinformation, promoting vaccine literacy, and building trust in vaccination programs. Clear and transparent communication about the safety and efficacy of vaccines is essential for addressing vaccine hesitancy.
- Enhanced Access to Vaccination Services: Ensuring equitable access to vaccination services, particularly in underserved or marginalized communities, is essential for improving vaccination coverage rates and reducing disparities in mumps susceptibility.
- Isolation and Quarantine: Implementing isolation and quarantine measures for individuals diagnosed with mumps and their close contacts helps prevent further spread of the virus within communities and congregate settings.
- Research and Development: Continued research into mumps epidemiology, vaccine effectiveness, and strategies for outbreak control is essential for informing evidence-based public health interventions and improving disease prevention efforts.
By addressing underlying challenges, promoting vaccine confidence, and implementing targeted interventions, public health authorities can effectively control mumps outbreaks and mitigate the impact of the virus on population health in the modern era.
The Future Research and Development
Current Trends in Mumps Research
Mumps research continues to evolve, focusing on various aspects of the virus, including its epidemiology, pathogenesis, and immunology. Some current trends in mumps research include:
- Genetic Diversity and Evolution: Studies investigating the genetic diversity and evolutionary dynamics of mumps virus strains aim to improve our understanding of viral transmission patterns and the emergence of new variants.
- Immune Response and Immunity: Research on the immune response to mumps infection and vaccination seeks to elucidate the mechanisms underlying protective immunity and vaccine-induced immunity, informing the development of more effective vaccines.
- Diagnostic Tools and Surveillance Methods: Advances in diagnostic tools and surveillance methods, such as molecular assays and serological testing, contribute to more accurate detection and monitoring of mumps cases, facilitating outbreak control efforts.
- Complications and Long-Term Effects: Research on mumps complications and long-term effects, including orchitis, oophoritis, and deafness, aims to identify risk factors, improve clinical management, and develop preventive strategies.
Potential Vaccines and Treatments in the Pipeline
Several potential vaccines and treatments for mumps are under investigation, with the goal of enhancing vaccine efficacy, improving treatment outcomes, and ultimately reducing the burden of mumps globally. Some promising avenues of research include:
- Next-Generation Vaccines: Novel vaccine platforms, such as virus-like particles (VLPs), recombinant subunit vaccines, and mRNA vaccines, offer the potential for improved immunogenicity, enhanced safety profiles, and simplified production processes compared to traditional live attenuated vaccines.
- Therapeutic Interventions: Antiviral drugs targeting specific stages of the mumps virus life cycle, as well as immunomodulatory therapies aimed at mitigating inflammation and immune-mediated tissue damage, represent potential treatment options for severe or complicated mumps infections.
- Vaccine Delivery Strategies: Innovative vaccine delivery systems, such as microneedle patches, mucosal vaccines, and needle-free injection devices, may improve vaccine acceptance, coverage, and delivery efficiency, particularly in resource-limited settings.
How Can We Eradicate Mumps Globally?
Achieving global mumps eradication presents significant challenges but remains an aspirational goal for public health efforts. Key strategies for eradicating mumps globally include:
- Universal Vaccination: Ensuring universal access to mumps vaccination, including routine immunization and catch-up campaigns, is essential for achieving and maintaining high population immunity levels necessary for mumps eradication.
- Sustained Surveillance and Response: Robust surveillance systems capable of detecting and responding to mumps outbreaks promptly are critical for preventing the reestablishment of transmission chains and maintaining progress toward eradication goals.
- International Collaboration: Collaborative efforts among countries, regions, and global health organizations are essential for coordinating vaccination strategies, sharing best practices, and mobilizing resources to address disparities in mumps control efforts worldwide.
- Research and Innovation: Continued investment in mumps research, including vaccine development, treatment modalities, and diagnostic tools, is crucial for advancing our understanding of the virus and improving the effectiveness of eradication strategies.
Conclusion & FAQs
In conclusion, mumps remains a significant public health challenge despite the availability of effective vaccines. The resurgence of mumps outbreaks in recent years underscores the importance of sustained vaccination efforts, public health awareness, and research into new preventive and therapeutic interventions. Vaccination remains the most effective strategy for preventing mumps and its complications, highlighting the importance of maintaining high vaccination coverage rates.
By staying informed, supporting vaccination efforts, and fostering international collaboration, we can work toward the goal of eradicating mumps globally and protecting the health of future generations.
Frequently Asked Questions (FAQs)
What are the common symptoms of mumps?
Common symptoms of mumps include swelling and tenderness of the parotid glands (located on the sides of the face), fever, headache, muscle aches, fatigue, and loss of appetite. Some individuals may also experience sore throat and difficulty swallowing.
How is mumps diagnosed?
Mumps is typically diagnosed based on clinical symptoms, particularly swelling of the parotid glands. Laboratory tests such as viral culture or polymerase chain reaction (PCR) may be performed on saliva, blood, or urine samples to confirm the presence of the mumps virus.
What are the complications associated with mumps?
Complications of mumps can include meningitis (inflammation of the membranes covering the brain and spinal cord), encephalitis (inflammation of the brain tissue), orchitis (swelling of the testicles), oophoritis (inflammation of the ovaries), and deafness. These complications are more common in adolescents and adults than in children.
Who should get vaccinated against mumps?
The Centers for Disease Control and Prevention (CDC) recommends routine vaccination with two doses of the MMR (Measles, Mumps, Rubella) vaccine for all children, starting at 12-15 months of age, with the second dose administered at 4-6 years of age. Adults who have not been vaccinated or who are unsure of their vaccination status should also receive the MMR vaccine.
Can mumps be prevented if I’ve been vaccinated?
While the MMR vaccine is highly effective, no vaccine provides 100% protection. However, vaccination significantly reduces the risk of contracting mumps and developing severe complications. In the event of exposure to mumps, individuals who have been vaccinated may experience milder symptoms and are less likely to develop complications compared to unvaccinated individuals. Regular booster doses of the vaccine may also be recommended in outbreak situations or for high-risk populations.

I do not even know how I ended up here but I thought this post was great I don’t know who you are but definitely you’re going to a famous blogger.